Operating Room Manners Class
Everything you need to know to feel comfortable and act normal on your first day in the operating room
If you didn’t have to go to cotillion as a kid, let me fill you in: it’s a traditional table manners and ballroom dancing class that parents of middle school kids in the South thinks builds character or something. Imagine: you’re 12 and your mom forces you to go to a stuffy ballroom after school where you don white cotton gloves, learn to distinguish between different kinds of forks, and then dance the foxtrot with random boys from your class (most of whom still have cooties).
Twelve-year-old me was awkward enough already. I didn’t need any extra-curricular humiliation!
After my own harrowing cotillion experience, it would be about another 15 years before I would encounter another circumstance so fraught with that same awkward mix of grandeur, interpersonal anxiety, and inscrutable social codes. Walking into the operating room as a med student for the first time brought it all rushing back.
The OR is a place like no other. It’s kind of a cult. To be generous, maybe it’s a secret society? It’s definitely a physical, mental, and emotional minefield.
The OR has about 500 rules that everybody seems to know, but nobody has bothered to write down.
So today, channeling my inner Miss (*ahem* DOCTOR) Manners, I’m here with Part 1 of my OR Survival Guide
You may have seen my Instagram series on “OR Manners” (linked below) but I wanted to pull everything together into a more organized, durable, and readily distributable handbook for budding OR nerds of all kinds. Read on, let me know what I missed, and send to somebody who could use the help!!
Let’s Set the Scene
Cast of Characters
Surgery is a team sport. Be respectful toward everybody, and try your best to avoid making assumptions about people’s roles. That is a classic faux pas.
Surgeon (duh) - If surgery is a dinner party, the surgeon is the host. You should introduce yourself to the surgeon before they scrub, and if you are a visitor/observer, ask if it is ok for you to stay (do not assume).
Anesthesiologist and/or anesthesia resident and/or CRNA - This is who is keeping the patient stable, asleep, and still during the operation. Patient safety is everybody’s priority, but it is the anesthesia team’s true raison d'être. During induction (aka when they are intubating/sedating the patient) they are running the room. You should be quiet and stay out of their way.
Circulator - This is who is running all of the logistics and documentation for the case. They stay un-scrubbed and solve any problems that come up along the way. They need to know who you are and how to spell your name so they can add you to the record.
Scrub - The captain of the sterile field. They manage the flow of the case and are responsible for making sure every instrument and supply is available when needed and accounted for at the end of the case. Whatever you do, do NOT mess up their counts.
Other critical people who will be in and out - OR charge nurse (this is the big boss and overseer of the whole OR kingdom, be extra nice), cleaning/turnover crew (essential to helping us expedite our day - try not to make their jobs harder), anesthesia tech (is often in the OR between cases getting things set up as part of the anesthesia team), various other OR managerial types.
Basic OR Geography
The sterile field - Assume that anything in the OR that is blue or on top of something blue is sterile. Do not touch blue unless you are also blue (aka sterile/scrubbed).
The back table - This is the larger of the scrub’s two work surfaces. This is where all of the instruments/supplies for the case are prepared and organized. Do not touch without asking.
The mayo stand - This is the smaller of the scrub’s two work surfaces, typically positioned across the patient during the case so that the scrub can easily hand things back and forth to the surgeon. You will feel tempted to touch it, or to grab something from it. Resist that urge. This is the scrub’s personal space.
Circulator’s desk/computer - This is not for you. The circulator needs unobstructed access to a computer at all times. Find somewhere else to sit.
Sterile core - Usually located in the middle of all the operating rooms. This is where all of the OR supplies are kept. If somebody asks you to go grab something, this is where it will be.
OR desk - This is the command center for all of the operating rooms. This is where the charge nurse will be. If you are lost, somebody here will help you.
Pre-op - This is where the patients get checked in before surgery. If you are early and looking to connect with the surgical team, they will likely be in this area greeting the patient, getting consent, marking, etc.
PACU - This is where the patients go to recover after surgery.
SNACK-U (aka lounge) - There is usually some area where the OR staff (and you!) can leave belongings, get a drink of water, have a snack, find a computer, etc.
Part 1: How to enter the OR like a civilized adult
Right place
If you can’t figure out where to go, ask around to find the OR desk. They will direct you.
When you’re getting close to the operating rooms, you’ll start seeing signs like “OR ATTIRE REQUIRED BEYOND THIS POINT.” These signs are serious, ignore at your own risk.
Once you enter the OR area, you will see boards or screens showing the schedule for the day and the status of each room. It’s sort of like the arrivals/departures board at an airport. Look here for the most up-to-date info about the day’s surgeries.
Right time
Get there early, before the surgery actually starts. Early means a minimum of 15 minutes before the scheduled case time. If this is your first day, remember that you will be navigating a new building, and that you will need time to change into scrubs and secure your belongings. Plan accordingly.
Right outfit
If you don’t have scrubs already, ask the OR desk for help.
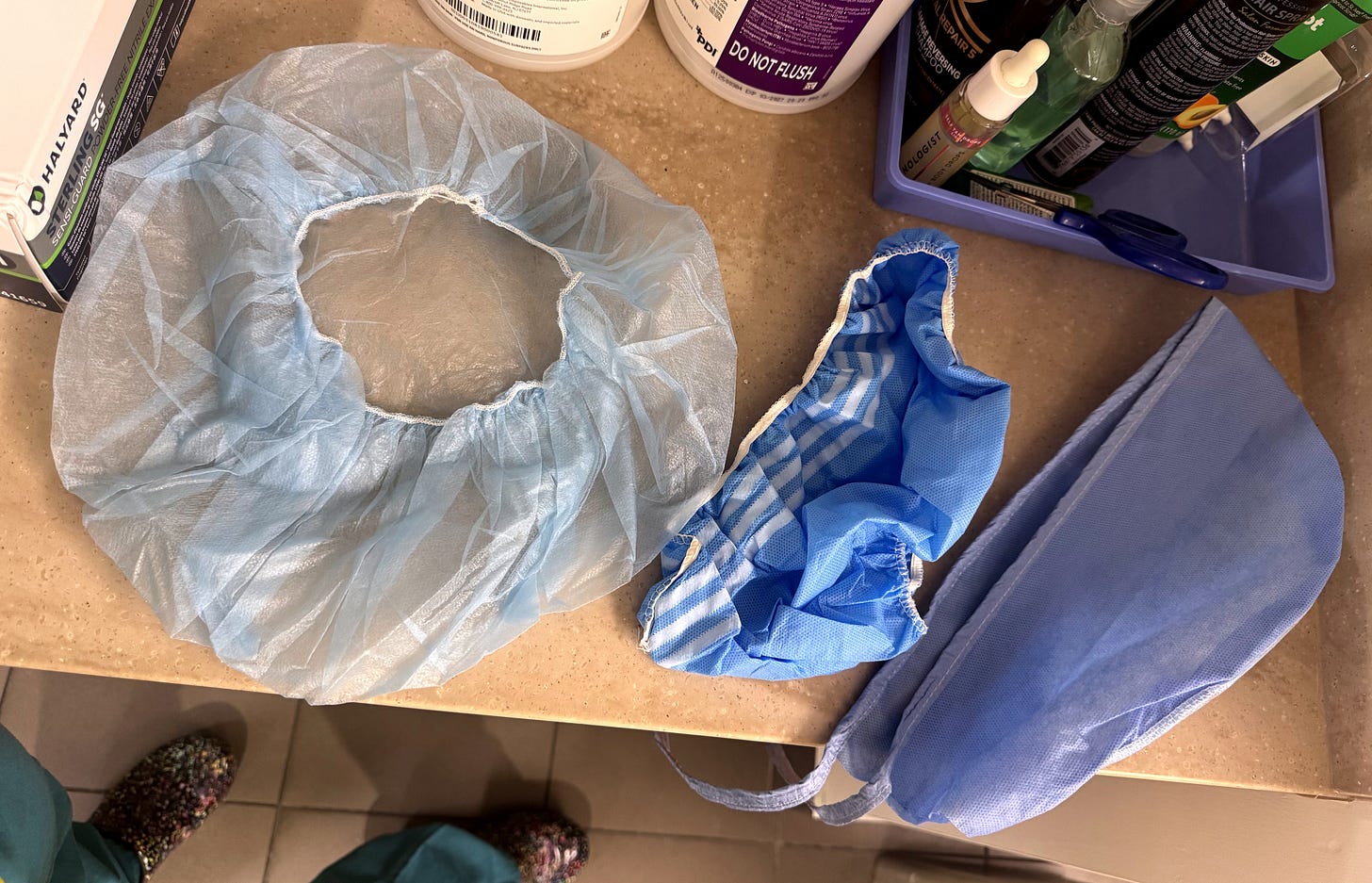
Required OR attire is typically scrubs, a scrub hat, and a mask. Hats and masks should be available at most entry points into the operating room area. The hat needs to cover all of your hair. If it has a tie or an extra elastic-y bit, that goes in the back. Do not put a shoe cover on your head, people will laugh.
Making a (subtle, appropriate) entrance
Enter the operating room and resist the impulse to lurk awkwardly against the wall waiting for somebody to notice you.
Approach whomever seems the least scary and introduce yourself like the eager adult learner you are: say hi, I’m Liz, I’m a student, and this is my first day in the operating room. What can I do to help?
Things you will likely be asked to do, and things that you should begin to do automatically as you get more comfortable:
Write your name on the white board. This is for two reasons: 1) it helps everybody keep track of who is in the room that day (it’s useful for you too when you forget the scary scrub tech’s name) and 2) the circulator needs to document everybody who is in the room, so this saves them from having to ask you how to spell your name later.
Get your gloves and offer to open them for the scrub. If you don’t know your size yet, ask somebody to help you figure it out. Most women wear 6 or 6.5, most men wear 7 or 7.5. If you know how to open your gloves steriley, ask the scrub if it is ok for you to drop your gloves on their table. Do not assume that it is ok, especially if you are new. If you don’t know how to open your gloves steriley, ask somebody to show you.
And just like that, you’ve made a good first impression as a med student who is on time, aware of their surroundings, and open to teaching and feedback! Next week, we’ll tackle the rules of the sterile field, how you can help with prepping and draping, and what you may be expected to do during and after surgery.
General Decorum
Use your eyes first, then your words, then your hands. You are learning to function in an environment where every little move you make matters. You are also surrounded by people who are watching you closely, deciding if they can trust you to behave in an appropriate, predictable way. There is a TON you can learn by watching: use your eyes without limit. The next safest thing is to use your words: ask questions, ask if it is ok for you to touch something or help with something, but if you are in any doubt about what to do or how to do it…ask before you use your fingers.
Let the attending lead the case AND the conversation. Some surgeons like to chat, some don’t. But for most every surgeon, there are times for talking and times for focusing. Until you have the experience to know the difference, err on the side of being quiet and deferential. Best times for questions? before the case, after the case, during closing/dressings, and when other people are already talking.
Adjust your personal space circumference. Surgery is close quarters. You will be touching other people at times, and not only the patient. You get used to it. Scooch in close enough so that you can see what’s happening. If you are too short, ask for a step stool.
Don’t sing or hum along to the music on your first day even if other people are doing it. Surgery karaoke rights are earned, not given.
Remember: not everything is about you. Even though you are here to learn and we are here to teach you, the patient is the focus and priority at all times in the operating room. If things get serious, shut up and stay out of the way.
Safety first: avoiding fainting and managing fatigue
The operating room is a perfect set up for a vasovagal episode. It’s hot, bright, crowded, there’s blood, and odds are you are dehydrated and hungry. The MOST important thing is to recognize if you are starting to feel faint, and to act to protect yourself by speaking up or sitting down/scrubbing out. If you fall, you become a second patient. Nobody’s got time for that.
Note: some people are also sensitive to colognes/perfumes…plz save these for the weekend
You will be standing in the OR for long periods of time. Your legs will get tired. When this happens, do not start doing leg stretch routines or take your shoes off (wouldn’t have to say it if it hadn’t happened). Appropriate strategies include: wearing compression socks, isometric exercises (tensing and relaxing your muscles without any disruptive body movement), and flexing/extending your toes INSIDE your shoes.

Pre-prep pit stop (aka all the things that happen before prep and drape)
When the patient arrives in the room, a LOT of things start happening all at once, and everybody is expected to pitch in. We confirm the patient’s identity/consent, move the patient from stretcher to bed, and make sure everything is ready to go for induction (aka anesthesia tube time). After induction, we make sure the patient is positioned safely and appropriately for surgery.
This is a great opportunity for med students to help out. Generally these are somegood, safe med student tasks:
putting on the squeezy boots aka sequential compression devices (SCDs)
fetching blankets from the blanket warmer
securing the patient’s safety strap
wheeling the stretcher back out into the hall
putting on the arm boards (this is harder than it looks, ask somebody to show you)
Now it’s time for induction. Stand to the side, be quiet, and let anesthesia do their thang.

Once the patient is asleep and the anesthesia team has taped or otherwise secured the tube you can help with:
exposing the operative site/removing extra blankets
positioning the arm boards, putting on arm straps, or tucking the arms
placing the bovie pad(s)
placing drip pads to prevent the prep solution from soaking into the linens
making sure that the prep solution is ready to go for whoever preps at your institution (this may be the scrub, the resident, the attending, or even you!)
Scrubbing In
This is one of those things that you just need somebody to show you how to do the first time, and then it will quickly become second nature. Briefly: scrub your hands the way your institution likes, walk into the OR keeping your hands above your waist, and let the scrub help you get your gown and gloves on. You are responsible for making sure the scrub has your gloves/gown before you scrub.
A quick-and-NOT-dirty summary of sterile technique:
Keep your hands in front of you, above your waist, and below your shoulders. You can rest them on the sterile field or keep them clasped in front of you. Don’t cross your arms or put your hands on your hips: your armpits aren’t sterile and neither are your hips.
Do not turn your back to any sterile surface (your back is not sterile either)
If you contaminate yourself or something on the field (aka a sterile person or thing touches a non-sterile person or thing) speak up immediately. You may need to re-scrub and whatever object got contaminated needs to be removed/addressed. Contamination happens to everybody, including attendings. It’s not embarrassing, you just need to be honest about it.
Don’t forget that there is a whole patient under those drapes. You’ll be surprised how easy it is to lose track of this fact. Don’t lean too heavily or rest your elbows on the patient. It’s rude and potentially injurious.
As a med student or junior resident, you generally want to scrub in either well before the attending (so you can help with draping), or just wait til after the attending is in so you don’t cause any delay. If you and somebody senior to you are both waiting to get scrubbed, let the senior person go first.
Draping/preparing the sterile field
This process is more nuanced than it looks. It is generally best to follow the lead of the scrub or resident/attending in a “monkey-see, monkey-do” fashion until you learn the ropes.
yes, you are the monkey in this scenario
Briefly, they will put blue drapes over everything that isn’t the operative field, and then set up a bunch of tools (bovies, suctions, scopes, lights, etc) that needs to be plugged in and at hand during the case.
OMG we’re finally there, surgery is happening!
Seeing a surgery for the first time is exciting and overwhelming. Keep in mind that the people around you do this all the time are having a totally different experience than you. They are participating in a lot of routinized behaviors, nonverbal communication, and social conventions that you don’t understand. Be a sponge, take it all in, and do what you’re told.
Things you may be asked to help with on your first day:
Retracting - imagine that you are made of thick, bendy wire so that you can be positioned in any pose and then you just stay exactly there until somebody moves you again. That’s the way you should retract (as a new person). Somebody will say “hold this,” and you just try to hold it exaaaactly where they have it without moving. The position of the retractor is more important than the amount of force you’re using to pull on it. Generally, you shouldn’t have to pull THAT hard. When they need you to move, they will move you.
If you need to let go/move for any reason, say something
Try to use your big muscle groups: stand up straight, keep your elbow adducted and activate your lats/traps for better endurance.
Cutting suture - This is a thankless task. Whatever you do, it’ll be too short, too long, or too slow. You’ll get better at it. Ask how long of a tail you should leave, and then just try to duplicate that length each time.
Hold your scissors like a surgeon, not like a child making a construction paper birthday card. Index finger on the screw, ring and thumb in the holes.
cut with just the tips of the scissors to avoid accidentally cutting anything behind the suture (it happens!)
Helping locate sponges or other objects - When there’s an incorrect count, this can be your moment to shine. It’s high stakes Where’s Waldo. Scour the field and the floor around you to see if you can find it and save the day.
Identifying anatomical structures - If your attending says “what’s that” and points at a blob or a string or something, just take a wild guess. Nobody expects you to get it right. But over time, you will learn to see stuff better and it’ll start to make sense.
The case is over! Now what
The case isn’t over ‘til the patient is safely to PACU
Resist the urge to immediately get lost in your phone once we break scrub: the drapes need to be removed and properly disposed, the patient needs to be cleaned of any remaining prep or blood, and, once the patient is extubated, the patient needs to be transferred back to a stretcher. All of these are excellent opportunities for you as a learner to help out.
Transferring the patient - this is a multi-person job with several important safety points to always keep in mind:
always confirm that the bed is locked before moving somebody. I just literally hip check it every time to make sure the brake is on.
all of the patient’s appendages and accessories (drains, foleys, lines, etc.) need to be free of entanglements and positioned safely prior to a transfer.
you need at least 4 people to safely move a patient: head, foot, and one for each side. Anesthesia always gets the head. If you are new, feet is the easiest and the best place to start. Watch how the two side people move the patient and then have somebody help you the first time you do that part.
As soon as they are transferred to the stretcher, get those side-rails up so the patient is safe and ready to move.
Traveling to PACU - you as the med student can help by steering the foot end of the bed on the way to PACU. Anesthesia gets the head. Stretchers usually have a steer mode but not everybody likes to use it/it doesn’t always work. Watch out for obstacles and watch your own fingers when going in and out of doorways and such.
Hat trick/handoff - any time a patient moves to a new place, you need to re-verify their identity and communicate with the new team what surgery the patient had and what the plan is going forward. In training settings the resident usually does this, but it’s something that more advanced med students do sometimes as well. As a student, just listen, pitch in if needed, and then look to your resident to see what’s next: either a break, done for the day, or if you’re lucky…on to the next case!
And just like that, you survived your first surgery!! You’ve made a good impression by being helpful at appropriate times, behaving predictably with patient safety as your priority, and you didn’t pass out (hopefully).
Some people come away from their first OR experience feeling like people are mean, or that they didn’t get to “do” anything. If that’s you, I would urge you to please give us another chance. There definitely are some rough personalities in surgery, but I think more often it’s just that the OR environment is intense and you have to earn a little trust at the outset before people open up. There’s no practice mode in surgery; it’s always a performance, and though people can seem casual, this is high-stakes serious business.
Don’t take it personally. Just show that you are paying attention and can follow directions. We’ll notice and start getting you more involved. You’ll be part of the team before you know it.
Thanks for reading!! And please share around. I was personally overwhelmed by my first OR experiences, and this is exactly the kind of guide I wish I’d had. Is there something important I missed??? Send me a message or let us know in the comments!